What Is an Atrial Septal Defect?
An atrial septal defect (ASD) is an abnormal opening in the tissue that separates the two top chambers of the heart. ASD is the most common birth defect found in children, according to the Texas Birth Defects registry.
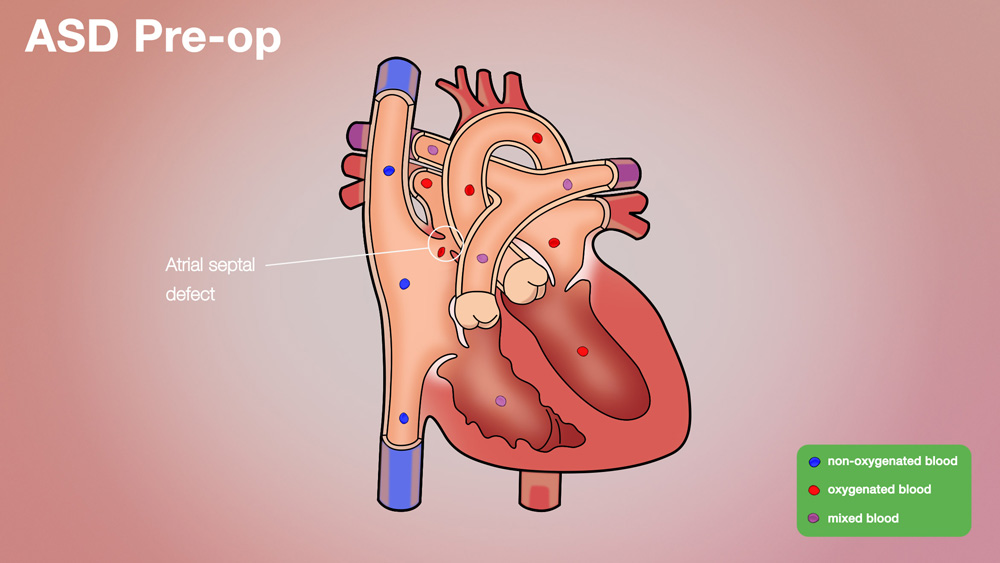
The heart has two sides: the right side of the heart pumps blood to the lungs to pick up oxygen, and the left side of the heart receives the oxygen-rich blood from the lungs and pumps it to the body. Each side has a main pumping lower chamber (ventricle) and a thin-walled upper chamber (atrium). Blood collects in the atria before filling each ventricle between beats. A thin wall, called the atrial septum, separates the left atrium from the right atrium. At various times when the baby is in the womb, there are holes in the wall (atrial septum), but by the time a baby is born, the gaps are nearly or fully closed. Remaining gaps are called atrial septal defects.
An ASD allows blood to flow across the defect, causing the ventricle to work harder. Blood will follow a path of least resistance when a hole exists in the atrial septum. The pressure in the lungs is lower than the pressure in the body; therefore in the presence of an ASD, blood will flow from the left atrium into the right atrium, which forces the right ventricle to work harder to move the excess blood through the lungs.
With a large ASD, the right ventricle may pump two to four times as much blood as the left side. Children rarely show any adverse effect from these efforts before their teenage years. Eventually, the extra work that the right ventricle has to perform takes its toll. The heart is like any other muscle, the harder it works the bigger the muscle gets. The heart muscle may also get stiff, and this makes it harder for the heart to effectively pump.
Approximately half of people beyond age 40 with an untreated, significant ASD will die due to heart failure. The attrition rate after age 40 is 6% yearly, as reported in Medscape Reference in 2015. Others may have a normal life span, but may be less active than they would be otherwise, may fatigue easily, and may become cyanotic (blue).
What Are the Causes of Atrial Septal Defect?
An ASD occurs if atrial septum gaps do not shut before birth. ASD is the leading birth defect in Texas, at 59 per 10,000 births, according to the Texas Birth Defects registry from data through 2011.
How Is Atrial Septal Defect Diagnosed?
About half of these defects close on their own, usually during childhood, according to the National Heart, Lung, and Blood Institute. Still, patients may have them for years, even decades, before they are detected. Issues such as labored breathing, abnormal heart rhythm, respiratory infections or pulmonary hypertension (high blood pressure in the heart and lungs) may lead to the discovery of an ASD.
Physicians may hear heart murmurs with a stethoscope and order further tests. The following tests may be utilized to find more details:
- An electrocardiogram (EKG or ECG), a painless exam, checks the heart’s electrical action to reveal damage or irregular rhythms suggestive of a laboring right ventricle.
- Chest X-rays create images of the heart and lungs, and the right side of the heart may be enlarged, suggesting an ASD.
- An echocardiogram (echo) uses sound waves (ultrasound) to produce images of the heart and vessels on a computer screen that reveals whether the heart is pumping properly, and can demonstrate an ASD.
- A cardiac MRI (magnetic resonance imaging) uses radio waves, magnets and a computer to form three-dimensional images of the heart, which can reveal structural abnormalities (such as an enlarged right ventricle) that an ASD can cause.Cardiac catheterization involves thin, long tubes, which are inserted into blood vessels and guided into the heart, with the help of fluoroscopy (X-ray).
What Are Atrial Septal Defect Treatment Options?
It is recommended that ASDs of significant size be closed. Since ASDs rarely become problematic until late childhood or young adulthood, doctors usually recommend atrial septal defect treatment when the child is large enough to make the closure easy but young enough such that symptoms are limited and the psychological trauma is minimized. Most ASDs are closed between the ages of two and five years.
Closure is very often performed through minimally invasive means in the cardiac catheterization suite. Specially-trained cardiologists insert a device into one of the large veins in the groin. A closure device is delivered in collapsed form through the veins to the site of the hole in the heart. It can then be expanded and placed into position to close the hole. In order to be closed with minimally invasive techniques, the holes must have a sufficient rim of tissue around them to seat the device. Otherwise, the holes must be closed surgically.
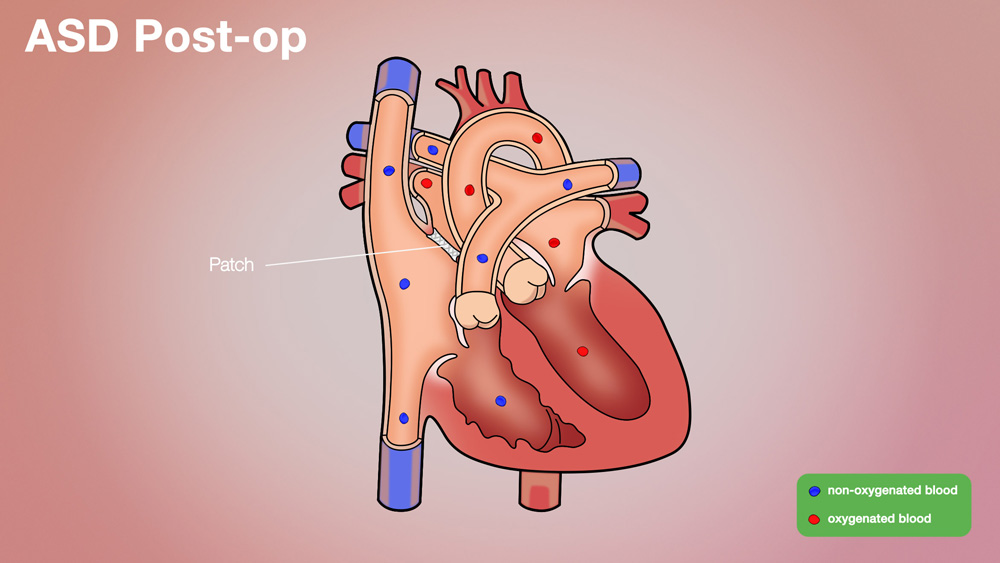
Surgical atrial septal defect treatment is performed by an open heart surgery, done using an up-and-down (vertical) incision in the midline of the chest. It is necessary to place patients on the heart-lung machine during surgery. Tubes are placed in the vessels coming back to the heart to draw blood away before it gets to the heart. The machine oxygenates the blood and pumps it back into the body. In this way, the surgeon can work inside the heart more easily. Closure of the hole involves sewing a small patch into place. A small incision is made in the right atrium to gain access to the ASD; the incision in the right atrium poses no damage to the heart. The child is then weaned off the heart-lung machine, the heart and lungs are allowed to take over the work of supplying oxygenated blood to the body, the chest is closed and the operation is completed.
What Are the Long-Term Effects?
An ASD closed in the cardiac catheterization lab requires a one-night stay in the hospital. Children who undergo surgical ASD closure usually stay in the hospital for 2-3 days. Rarely do children have any long-term adverse effects.
What Follow-Up Care Is Needed?
Patients who have an ASD closed in the cardiac catheterization lab will take aspirin once a day for six months to prevent blood clots from forming. They will need to follow up in clinic with a pediatric cardiologist regularly, and will have the heart and device assessed with echocardiograms. They can resume most normal activities soon after the procedure.
Patients who have an ASD closed as a surgical procedure will follow up with the surgeon about 2 weeks after discharge and will see their pediatric cardiologist 3-4 weeks after discharge. Activity is limited for 6-8 weeks after surgery due to the sternal bone healing, but after that time, there are little if any restrictions placed.
Why Choose the Children’s Heart Institute?
At Children’s Heart Institute at Children’s Memorial Hermann Hospital, patients with congenital or acquired heart disorders receive hands-on specialized care 24/7 from a team of affiliated physicians and specialty-trained nurses who aim to deliver the best possible outcomes.
Children’s Memorial Hermann Hospital was named one of the top children's hospitals nationally in Cardiology & Heart Surgery by U.S. News & World Report. In addition, Children’s Heart Institute is among the top congenital heart surgery programs in North America for patient care and outcomes, according to the Fall 2019 Society of Thoracic Surgeons (STS) Congenital Heart Surgery Database Report of 118 STS participating programs.
In collaboration with various subspecialties, the affiliated team provides comprehensive care for newborns, children and adolescents, with the ability to transition into adult congenital cardiac care. Team members have the experience and skills necessary to offer innovative treatment methods and specialized services, including, but not limited to:
- Biventricular repairs and biventricular conversions
- Congenital heart optimization
- Full repairs for complex congenital heart defects in newborns
- Hybrid catheterization and surgical procedures
- Minimally invasive transcatheter pulmonary valve (TPV) therapy
- Minimally invasive repairs
- Treatment for adult congenital heart disease
- Valve repairs and preservation
With the Level IV Neonatal Intensive Care Unit (NICU) and a dedicated Children’s Heart Institute Intensive Care Unit at Children’s Memorial Hermann Hospital, critical heart patients have access to quality, specialized care. By utilizing state-of-the-art techniques, the team at Children’s Heart Institute strives to offer patients with the most complex problems the greatest opportunity for a normal life.
Contact Us
If you have any questions, use the online tool below to help us connect with you. To refer a patient or schedule an appointment, please contact our clinic using the information below.
- Pediatric Cardiology Clinic
The University of Texas Health Science Center Professional Building
6410 Fannin, Suite 370
Houston, TX 77030
Phone: (713) 486-6755 (Appointment Line)
- Pediatric and Congenital Heart Surgery Clinic
The University of Texas Health Science Center Professional Building
6410 Fannin, Suite 370
Houston, TX 77030
Phone: (713) 500-5746
CMHH-Heart@memorialhermann.org
To contact Children’s Heart Institute at Children’s Memorial Hermann Hospital, please fill out the form below.
The Children’s Heart Institute is a collaboration between the affiliated physicians at McGovern Medical School at UTHealth Houston and Children’s Memorial Hermann Hospital. Typically, patients are seen on an outpatient basis at a UT Physicians clinic with all inpatient procedures performed at Children’s Memorial Hermann Hospital.