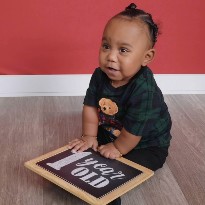
Landon's Journey: Overcoming CDH with Gratitude and Hope
April 17, 2024
When Elizabeth came in for a second scan a week later, things felt off. The ultrasound technician kept going back to the same spot, muttering about the baby's diaphragm. Finally, she broke the silence with, "I can't see his diaphragm. It's there... and then it stops. I need to contact your OBGYN....